Like the Hydra of Greek myth, cancer is a many-headed beast. The disease not only manifests in different parts of the body but also varies in how it responds to the same treatments. Clinicians often must choose between ‘scorched earth’ options that burn through both healthy and cancerous cells, versus more targeted therapies that work well on only a few cancer types.
An unconventional new class of drugs might balance both outcomes. In a recently concluded phase 2 clinical trial, an international team led by Qi Zeng, Research Director at the A*STAR Institute of Molecular and Cell Biology (A*STAR IMCB), demonstrated that PRL3-zumab—the first-in-class humanised antibody drug designed to target intracellular PRL3 proteins—can extend the progression-free survival (PFS) of patients with late-stage IV cancers of multiple types.
“PRL3-zumab has the potential to be a safe broad-spectrum anti-cancer drug, as the PRL3 protein is highly (about 80.6 percent) expressed in a wide range of cancers, but undetectable in healthy tissues,” said Zeng.
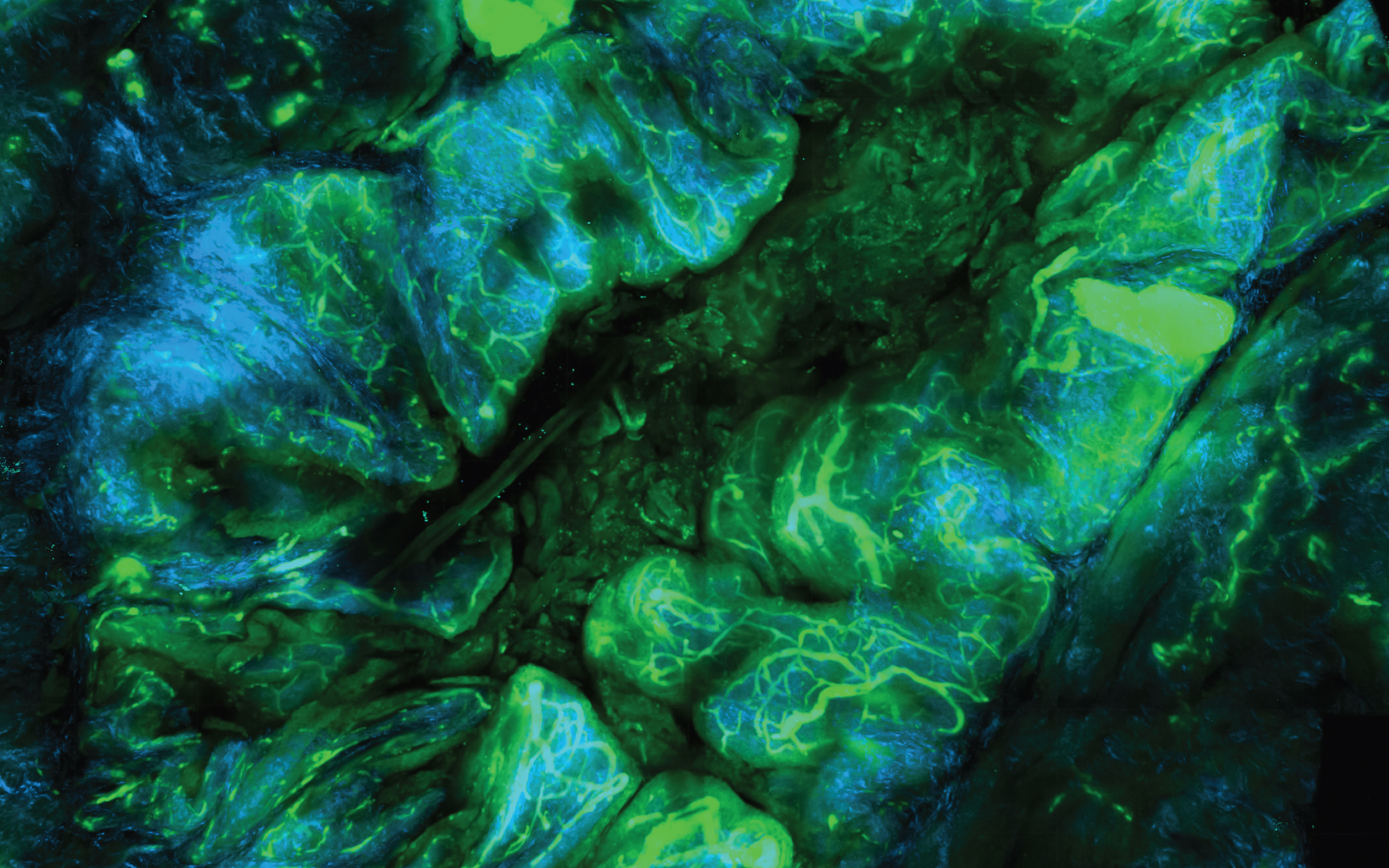
First discovered by Zeng and colleagues in 1998, PRL3 is typically buried inside cancer cells, making it unreachable by antibodies. Later research revealed that PRL3 can ‘flip’ onto the cancer cell surface under the harsh tumour microenvironment, exposing it as a druggable target. This insight led to PRL3-zumab, which showed an excellent safety profile in a 2018 phase 1 clinical trial at the National University Hospital, Singapore.
For the drug’s phase 2 trial, Zeng and A*STAR IMCB colleagues, including Senior Scientist Min Thura, collaborated with the National Cancer Centre Singapore and multiple cancer research institutes in the US, China and Malaysia. The US trial was approved by the US Food and Drug Administration (FDA) and sponsored by the A*STAR spinoff biotech company Intra-ImmuSG, which Zeng founded.
The trial evaluated 51 patients across a ‘basket’ of cancer types, including gastric, anal, lung, colon, cervical, ovarian and kidney cancers. Zeng noted that the challenges of the COVID-19 pandemic meant that most enrolled patients had late-stage cancer with a limited runway to evaluate drug efficacy.
To address this, the team used a novel analytical method called Single Evaluable Patient Single Cohort (SEPSC) to draw insights from the study’s small yet diverse sample size. SEPSC compared each patient’s PFS—defined as length of time without cancer progression—against both historical PFS data from existing treatments (external controls), and the patients’ own outcomes on previous treatments (internal controls).
The team found that patients treated with PRL3-zumab survived significantly longer without disease progression, with only mild and few side effects. Zeng also highlighted that ongoing trials enrolling patients with sarcoma, nose and kidney cancers, and aggressive small cell lung carcinoma—conditions with few standard-of-care treatment options—showed promising responses to the drug.
“PRL3-zumab could bring new hope for patients with hard-to-treat cancers by significantly extending their PFS,” said Zeng. Spurred by these findings, the team is pursuing FDA conditional drug approval for PRL3-zumab via a breakthrough fast-track pathway for treating sarcomas, addressing urgent unmet needs for patients with no remaining treatment options.
The A*STAR-affiliated researchers contributing to this research are from the A*STAR Institute of Molecular and Cell Biology (A*STAR IMCB).