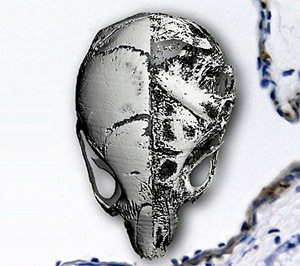
Composite image showing the skull of a normal mouse (left) and a mouse with progeria (right). Background image is a section from the pulmonary artery of a progeric mouse, showing extensive apoptosis (brown staining) in the vascular smooth muscle.
Hutchinson–Gilford progeria syndrome (HGPS) is a rare genetic disease that affects one in every 4–8 million newborns. Children with HGPS appear normal at birth, but develop symptoms of aging, including growth retardation, skin wrinkles, hair loss and fragile bones, within the first 12 months. There is no known cure for HGPS, and few children with HGPS ever reach the age of 13—90% of them die from complications of atherosclerosis, such as heart attack or stroke.
Genetic studies have shown that HGPS is caused by mutations in the gene LMNA. In 2003, Colin Stewart and co-workers at the A*STAR Institute of Medical Biology and the National Cancer Institute in the USA reported an LMNA-mutated mouse line that exhibits a variety of HGPS symptoms. Seven years later, the same group has used the mouse line to reveal the molecular etiology and pathology of HGPS.
Fibroblasts are cells responsible for synthesizing the extracellular matrix (ECM) of connective tissues and collagen in skin cells. The researchers compared fibroblasts obtained from LMNA-mutated mice at embryonic day 13 with those obtained from LMNA-mutated mice at postnatal day 14–21. They observed proliferation arrest and cell death in postnatal, but not embryonic, fibroblasts.
The researchers also compared the gene expression and growth of LMNA-mutated mice with those of normal mice. They found that LMNA-mutated mice had reduced ECM and cell adhesion gene expression, as well as abnormal skeletal and vascular development. The findings suggest that mutations in LMNA cause problems in postnatal development by altering ECM and cell adhesion gene expression, which in turn, affect skeletal and vascular maintenance.
A question raised by these findings is how mutations in LMNA, a gene responsible for encoding nuclear envelope proteins, can have such large effects on the cell membrane and ECM. The researchers therefore analyzed all the signaling pathways that might potentially be affected and found that mutations in LMNA could inhibit the canonical Wnt signaling pathway by reducing nuclear localization and transcriptional activity of Lef1.
Defects in canonical Wnt signaling could cause problems in ECM synthesis. The finding suggests that HGPS is a disease of the ECM and connective tissue and that there may be therapeutic targets in the canonical Wnt signaling pathway for HGPS.
“Our findings may also provide insights into how arthrosclerosis develops, as a consequence of vascular smooth muscle defects, during aging,” says Stewart.
The A*STAR-affiliated researchers contributing to this research are from the Institute of Medical Biology.



