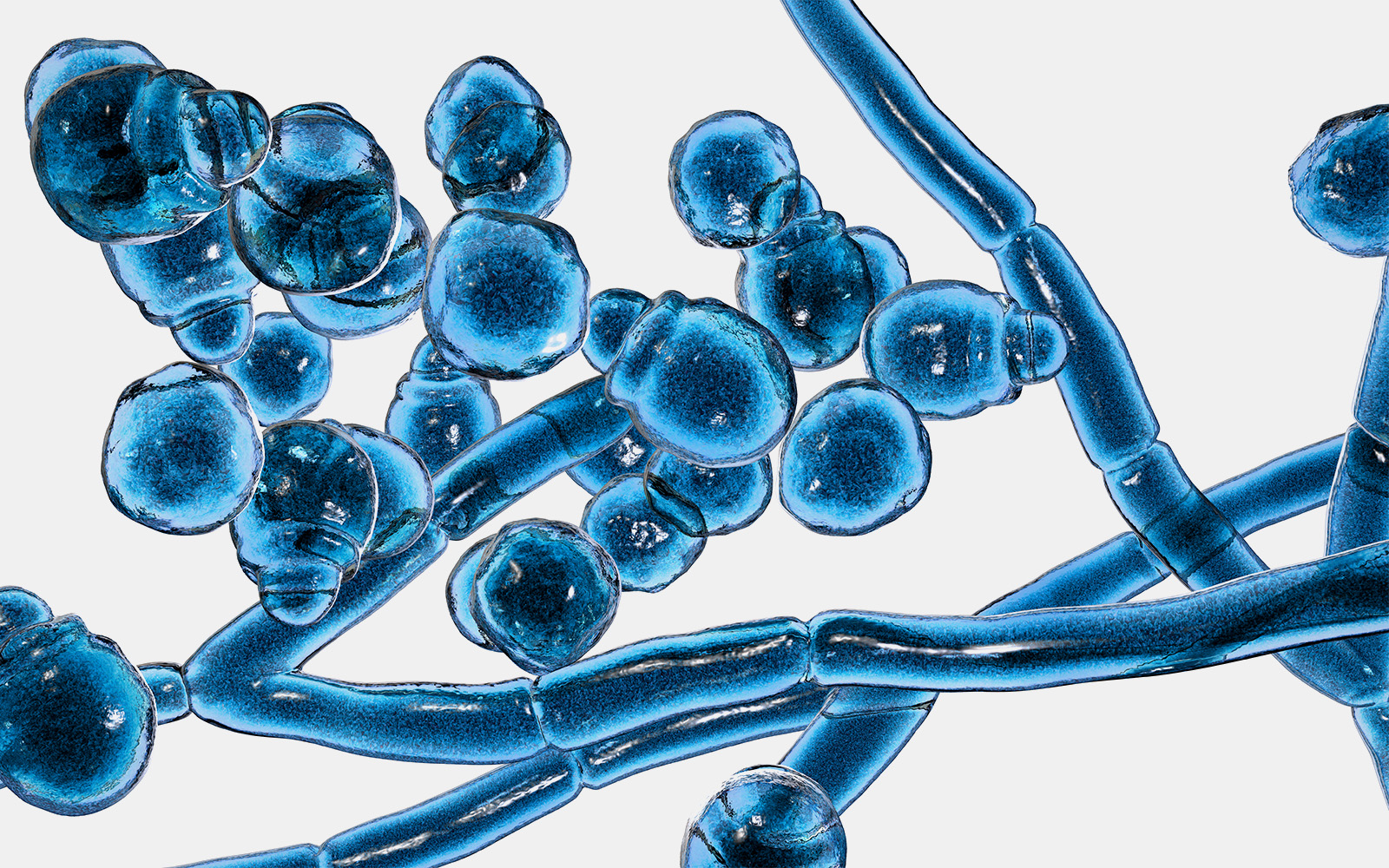
We often think of our skin’s microbiome as predominantly bacterial. Surprisingly, yeast such as Malassezia also thrive on warm, moist, greasy and nutrient-rich human skin. While typically harmless, Malassezia can sometimes flip from friend to foe, triggering dermatological conditions from dandruff to dermatitis.
“In individuals with healthy skin, the skin barrier is usually intact, which allows the skin to function properly as a protective barrier defending against the external environment,” said Thomas Dawson, Deputy Executive Director at the A*STAR Skin Research Labs (A*SRL).
Dawson explained that when this barrier is compromised, Malassezia can infiltrate into deeper layers of skin where they secrete many compounds including protein-digesting enzymes called proteases, which lead to itchy, inflammatory flare-ups.
Historically, researchers have encountered hurdles in trying to connect the dots between protease genes and the exacerbation of skin conditions—the yeast is difficult to genetically modify and grow in the lab for experimental analyses. Using a novel approach, Dawson teamed up with collaborators from the National University of Singapore; National Skin Centre, Singapore; University of California San Diego, USA; and the University of Zürich, Switzerland to study the gene expression profiles of Malassezia furfur, a more experimentally accessible model organism for studying the yeast’s impact on skin health.
First, the team took skin samples from patients with atopic or seborrheic dermatitis, alongside healthy volunteers. Gene expression analyses revealed that individuals with dermatitis showed a marked uptick in the expression of MGSAP1, a protease gene.
The researchers then disabled a similar yeast gene called MFSAP1 in M. furfur and observed changes in the way the yeast cells stick together and grow on lab-grown human skin. They found that the absence of MFSAP1 in a mouse model resulted in significantly less skin inflammation, as indicated by reduced swelling and fewer inflammatory cells, compared to the wild-type M. furfur. This confirmed the team’s hypothesis that the Mfsap1 protease is involved in the host inflammatory response.
“Mfsap1-mediated modifications of the cell surface and the external environment can enable the fungal cells to become more hydrophobic, contributing to a shift from free-floating to adherent cells,” explained Joleen Goh, the first author of the study.
Goh added that these newly gained insights explain how the yeast interacts with the skin environment, which can enable targeted treatments for inflammatory skin conditions.
“Future treatment of Malassezia-associated conditions can be coupled with enzyme inhibitors and antimycotics in controlling infections to improve clinical outcomes,” Dawson and Goh suggested, adding that their group plans to study how M. furfur attaches to medical devices like catheters, which is particularly dangerous for high-risk patients such as new-borns and the immunocompromised receiving lipid emulsions.
The A*STAR-affiliated researchers contributing to this research are from the A*STAR Skin Research Labs (A*SRL), Bioinformatics Institute (BII) and the Institute of Molecular and Cell Biology (IMCB).