When ocean tides retreat, sea creatures can sometimes get trapped in pools on the rocky shore. Similarly, SARS-CoV-2—the virus responsible for the COVID-19 pandemic—can sometimes persist in the body long after symptoms subside, leaving the resident immune cells activated in a state of high alert.
Joe Yeong, Group Leader at A*STAR’s Institute of Molecular & Cell Biology (IMCB), said that this phenomenon may have important implications for patients undergoing cancer treatments that target the immune system. “What concerns us is that the tumour immune microenvironment can alter the efficacy of cancer treatments such as immunotherapies.”
Together with Mai Chan Lau, a Senior Researcher at A*STAR’s Bioinformatics Institute (BII) and IMCB Senior Research Officers Denise Goh and Jeffrey Lim, Yeong’s team forged a collaboration with international researchers involved in the Long Covid Autonomous Communities Together Spain (LongCovidACTS) study as well as researchers from the Duke-NUS Medical School, National Cancer Centre Singapore and Singapore General Hospital.
Through this programme, the team gained access to appendix, skin, and breast tissue samples from two patients who were diagnosed with long COVID. Despite testing PCR negative for SARS-CoV-2, these patients exhibited prolonged and persistent symptoms 163 and 426 days after the infection’s acute phase.
Using spatial transcriptomics (ST), a sequencing technology that tracks changes in gene activity in intact tissues, the scientists aimed to gain insights into how tumour-associated immune cells might behave differently due to residual SARS-CoV-2.
“ST can detect tens of thousands of genes at one go from the same tissue section,” remarked Yeong, who added that the technique can also detect the presence of viral genes.
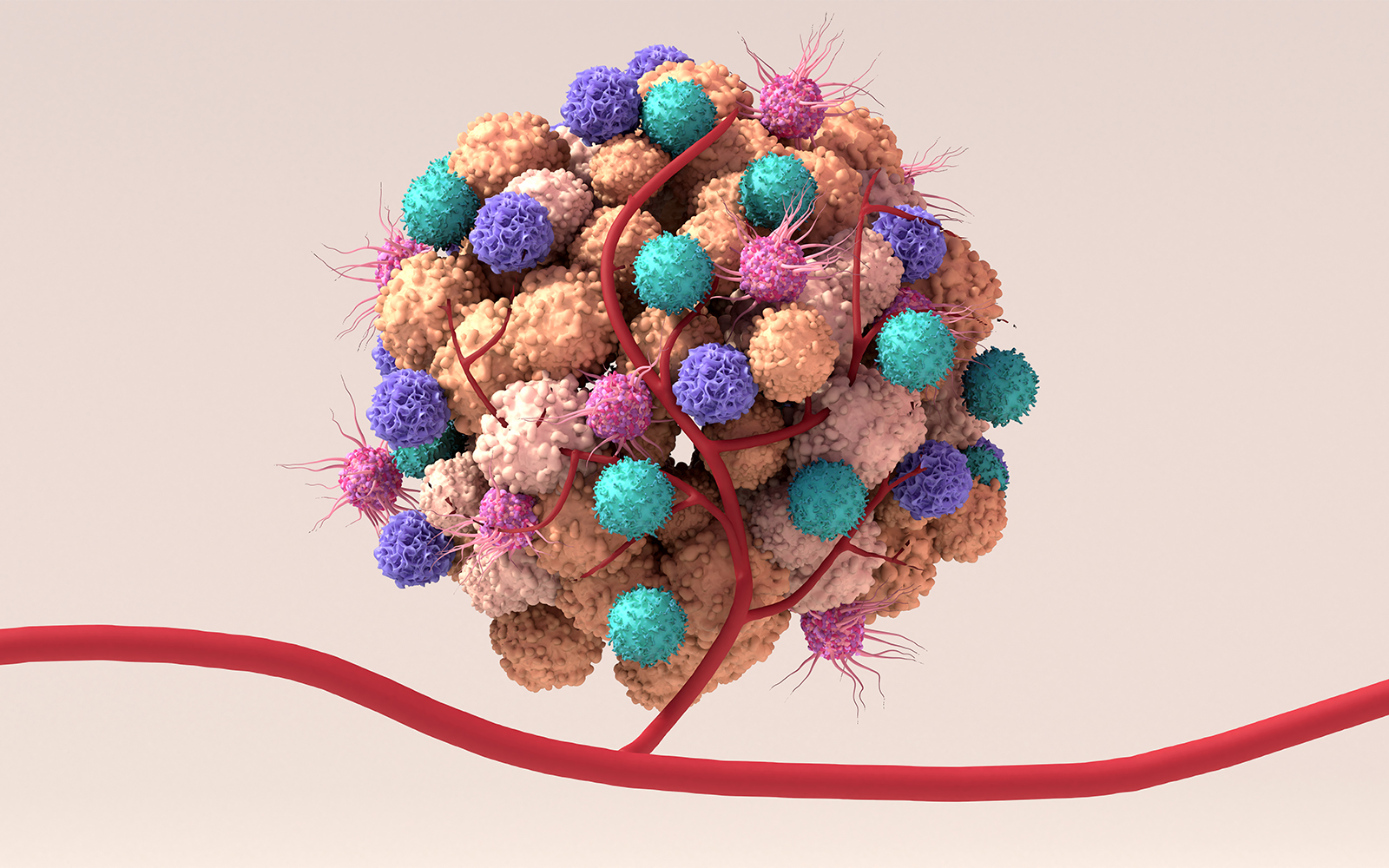
With liver and colon cancer patients who had previously recovered from COVID-19, the team's analysis revealed active antibody-producing B cells in tissues with traces of SARS-CoV-2, which included the periphery of tumours. The gene activity in these immune cells suggested that an active defence response was still in progress.
Next, they investigated whether this buzz of activity might alter the degree of a tumour’s response to immunotherapy. The team generated predictive scores based on changes to immune gene activity. Surprisingly, they found that tumours harbouring viruses could be more susceptible to the effects of immunotherapy.
The researchers hypothesised that a localised uptick in tumour-killing cells such as T cells and cytotoxic lymphocytes could potentially enhance the therapeutic effects of such cancer treatments.
According to Yeong, population-level studies could help clinicians hone in on cancer patients with long COVID who might respond better to immunotherapy. “I believe the findings have a huge impact on our understanding of virus-driven cancers such as some forms of liver, nose and cervical cancers,” concluded Yeong.
The A*STAR-affiliated researchers contributing to this research are from the Institute of Molecular & Cell Biology (IMCB) and Singapore Immunology Network (SIgN).