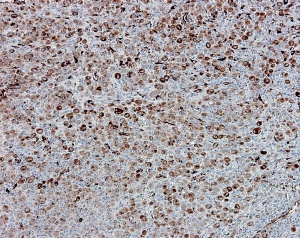
A microscopic image of melanoma tumor cells expressing SPARC
From Ref. 1 © 2011 A. Nardin
Melanoma is a form of skin cancer which is curable if treated early enough. Advanced melanoma is often treated with the tumor cell-killing drug dacarbazine, but only a few tumors respond to the treatment. Understanding why chemotherapy induces tumor shrinkage in some patients but not others is essential to improve therapeutic treatment. Now, an international team of researchers, including groups from the Singapore Immunology Network and the Bioinformatics Institute at A*STAR, have identified gene expression changes that are linked to a beneficial response to dacarbazine in melanoma patients.
The researchers obtained melanoma lesions from 13 patients both before and after treatment with dacarbazine, and examined the genes that were expressed in those lesions. A small subset of those lesions appeared to respond to the drug, either by shrinking or by stopping their growth. From this analysis, the team could observe which types of genes tended to be expressed in the lesions that responded to the drug, and could therefore identify the cellular processes that were linked to a beneficial outcome in the patients.
The extracellular matrix (ECM) is a network of proteins found on the outside of cells that maintains their arrangement and organization. The researchers found that the expression of genes involved in ECM remodeling, such as secreted protein acidic and rich in cysteine (SPARC), is increased in melanoma lesions that responded to dacarbazine (see image), but not in lesions that did not respond to the drug. Immune cell infiltration into tumors can indicate the activation of an immune response, which can contribute to cancer eradication. The team observed that the expression of genes and proteins linked to immune cell invasion and activation, such as tumor necrosis factor (TNF) and CD8, were upregulated in melanoma lesions that responded to dacarbazine, but were unchanged or decreased in lesions that did not respond.
Patients whose melanoma lesions experienced increases in the expression of genes linked to the immune response or to ECM remodeling tended to live longer than patients whose tumors did not exhibit these changes. “Scientists previously hypothesized that the mechanism of action of chemotherapy may not be limited to direct toxicity on tumor cells, and we demonstrate here for the first time that this is indeed the case for dacarbazine,” explains Alessandra Nardin, the first author of the paper.
The findings can aid in the understanding of how to combine other therapies, such as immune cell transfer, with dacarbazine to boost the beneficial response it can elicit in melanoma patients.
The A*STAR-affiliated researchers contributing to this research are from the Singapore Immunology Network and Bioinformatics Institute.



